Breast development is a normal part of growing up, but it rarely feels simple. Some girls feel early, others feel late, and many notice one side leading the other. Dr. Michael Baumholtz explains these changes in clear, practical terms so families understand what is typical, what can vary, and when a medical visit makes sense. His aim is education, steady reassurance, and practical next steps - never pressure or promises.
Video: How To Pick Breast Implants
Quick Facts
Most people notice the first changes between ages 8 and 13, often as a small, tender bud beneath one or both nipples. Growth tends to arrive in spurts rather than in a straight line, and left-right differences are common while one side temporarily leads the other. For many, puberty-driven changes slow toward the end of high school and settle by 17 to 18, with subtle refinements into the early 20s as monthly cycles stabilize. Later shifts in size or feel are usually tied to weight change, pregnancy and breastfeeding, contraception, or menopause. It is sensible to check in with a clinician for very early signs before age 7 to 8, no breast budding by about 13, a hard or fixed lump, persistent discharge, rapid one-sided growth, or concerning skin changes.
What This Page Covers
This page describes what clinicians mean by normal breast development, how timing varies from person to person, and how to recognize when puberty-driven growth has mostly finished. It addresses left-right differences, the influence of weight, hormones, pregnancy, and menopause, and when to see a medical professional. It also outlines how Dr. Baumholtz discusses aesthetic options after growth is complete, with attention to proportion, tissue quality, and long-term planning rather than cup size targets.
Understanding Normal Breast Development
Breast development is guided by hormones - mainly estrogen and progesterone - and unfolds over several years. The first sign for many is a firm, sometimes sensitive nodule beneath the nipple and areola, known as thelarche. One side often starts first and the other follows months later. Other puberty markers typically appear around the same time, including pubic and underarm hair, a height spurt, and, usually two to three years after breast budding, the first menstrual period. Soreness and fullness can ebb and flow across months, which is a normal pattern rather than a problem.
The Tanner Stages - The Medical Road Map
Clinicians often describe development with five Tanner stages. Stage 1 is prepubertal with no true breast tissue. Stage 2 is the breast-bud stage as a small mound forms beneath the nipple and areola. Stage 3 brings noticeable enlargement and a fuller contour. Stage 4 can show the areola and nipple as a secondary mound above the rest of the breast. Stage 5 reflects an adult pattern in which the areola usually blends with surrounding skin and projection is mainly at the nipple. The ages attached to these stages vary widely and do not, by themselves, indicate a problem.
When Do Breasts Usually Stop Growing?
There is no single date when growth ends, but there is a reliable window. Most puberty-related change happens in the teen years. Toward the end of high school, growth slows, and by 17 to 18 many people find their size and shape are fairly consistent. Some notice modest adjustments into the early 20s as cycles and body composition settle. Beyond that, changes tend to reflect life events rather than puberty.
Practical Clues Growth Is Mostly Done
Growth has usually settled when bra size is stable for a year or two, height has plateaued, and menstrual cycles have been regular for a couple of years. If changes occur later on, they usually track to specific events such as weight change, pregnancy and breastfeeding, or starting and stopping hormonal contraception rather than ongoing pubertal development.
What Shapes Size And Appearance?
Size and shape reflect genetics, hormones, and body composition. Family traits can suggest a general direction, though each person’s outcome is individual. Estrogen and progesterone drive development of the glandular structures and influence how much fat becomes part of the breast. Because breasts contain fat, overall weight shifts often change cup size and contour. Some medications and hormonal birth control can create temporary fullness for certain people, usually from fluid balance and small weight changes, and those effects often settle with time. Very low body fat, as seen in high-level athletics, can delay timing or limit size. Routine exercise and a supportive bra improve comfort without altering the biology of development.
Asymmetry - When One Side Leads
Left-right differences are the rule rather than the exception, especially during puberty when one breast may begin earlier or grow faster. Most differences narrow with time or settle into a mild mismatch that is obvious mainly to the person themselves. Seek medical review if change is very rapid on one side, if a lump feels unusually firm or fixed, if discharge is persistent and bloody or clear, or if the skin looks dimpled, puckered, red, or warm. After growth is complete and health causes are excluded, Dr. Baumholtz can discuss ways to improve balance. Options can include a small reduction on the larger side, a small implant on the smaller side, or selective fat transfer to soften edges. The goal is balance that respects tissue limits and long-term maintenance.
Normal Changes After Puberty
Across adulthood, breasts continue to respond to physiology and life. Many people feel fuller and more tender in the days before a period, then more relaxed afterward. Pregnancy and breastfeeding expand the glandular system, stretch the skin envelope, and can leave the breasts a different size or position than before. Significant weight change alters volume and the distribution of fullness. Around menopause, glandular tissue shrinks and fat often contributes more to volume, changing density and feel. These transitions are normal and do not represent a second round of puberty.
When To See A Medical Professional
Most differences fall within a broad normal range, but some patterns deserve timely evaluation. Signs of breast development well before age 7 to 8 should be assessed for early puberty, and the absence of breast budding by about 13 is usually evaluated for delayed puberty. At any age, a new hard or fixed lump, persistent bloody or clear discharge, redness and warmth that suggest inflammation, or rapid one-sided enlargement should prompt a visit with a clinician. A pediatrician, primary care doctor, gynecologist, or adolescent medicine specialist is the appropriate starting point. Plastic surgery discussions come later, after health questions are resolved and growth appears stable.
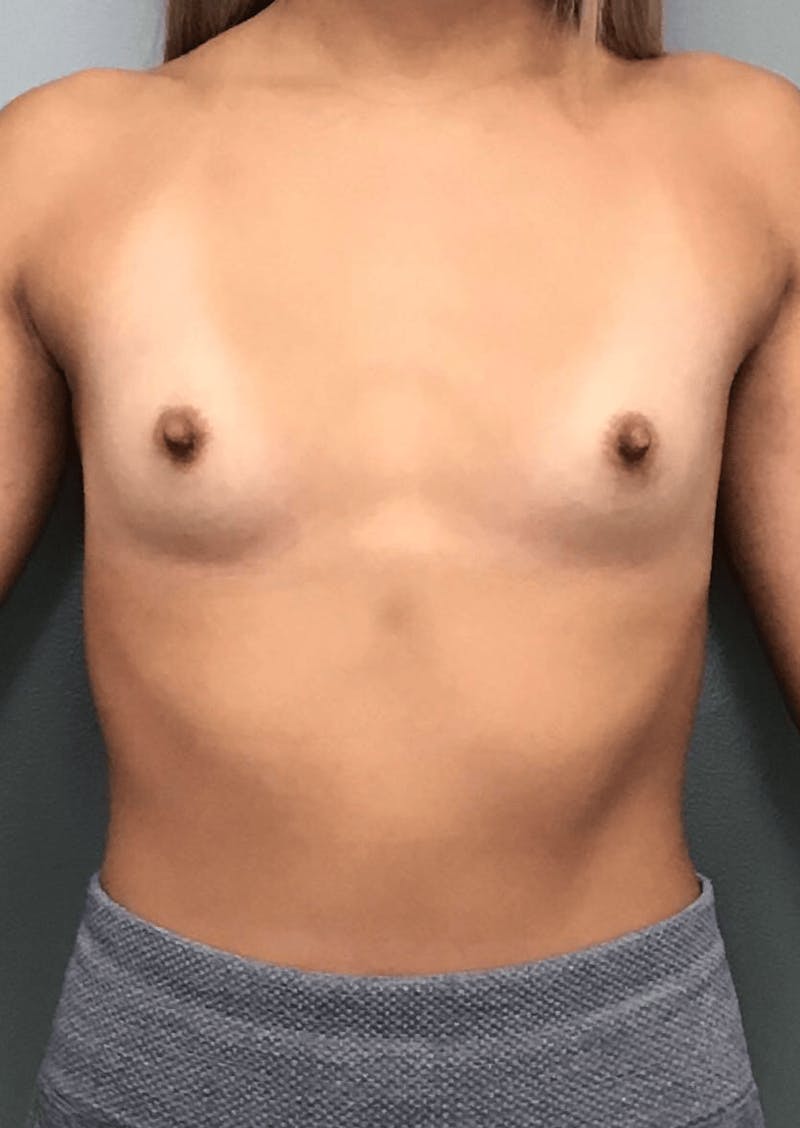
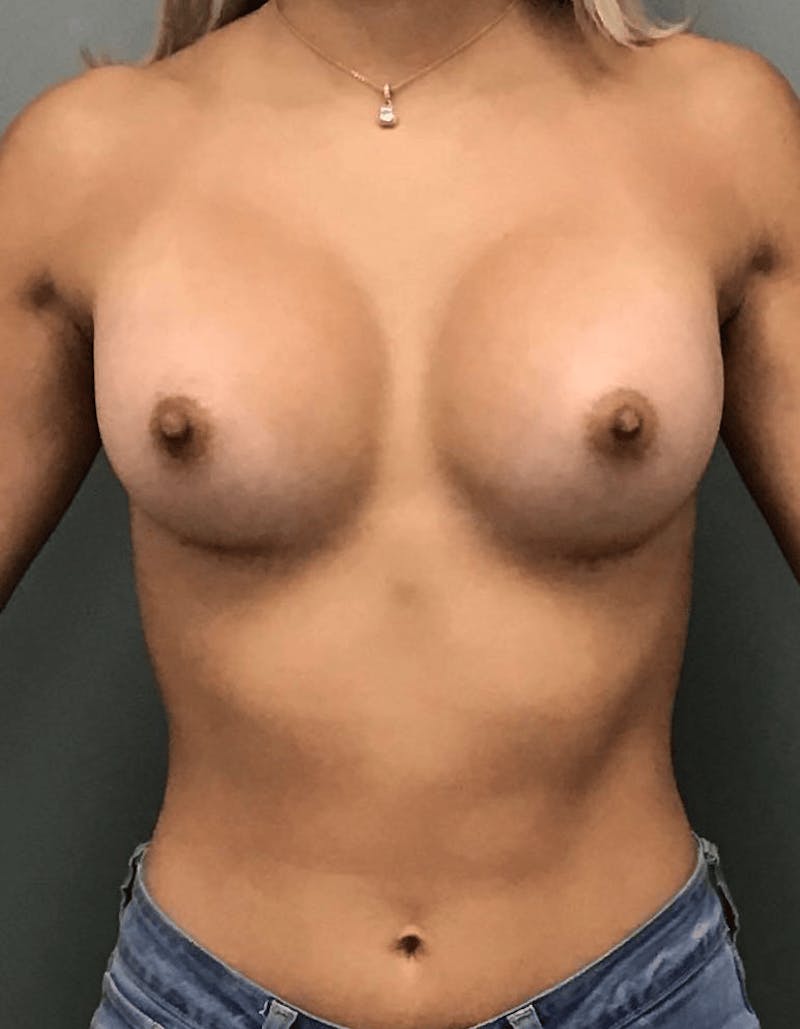
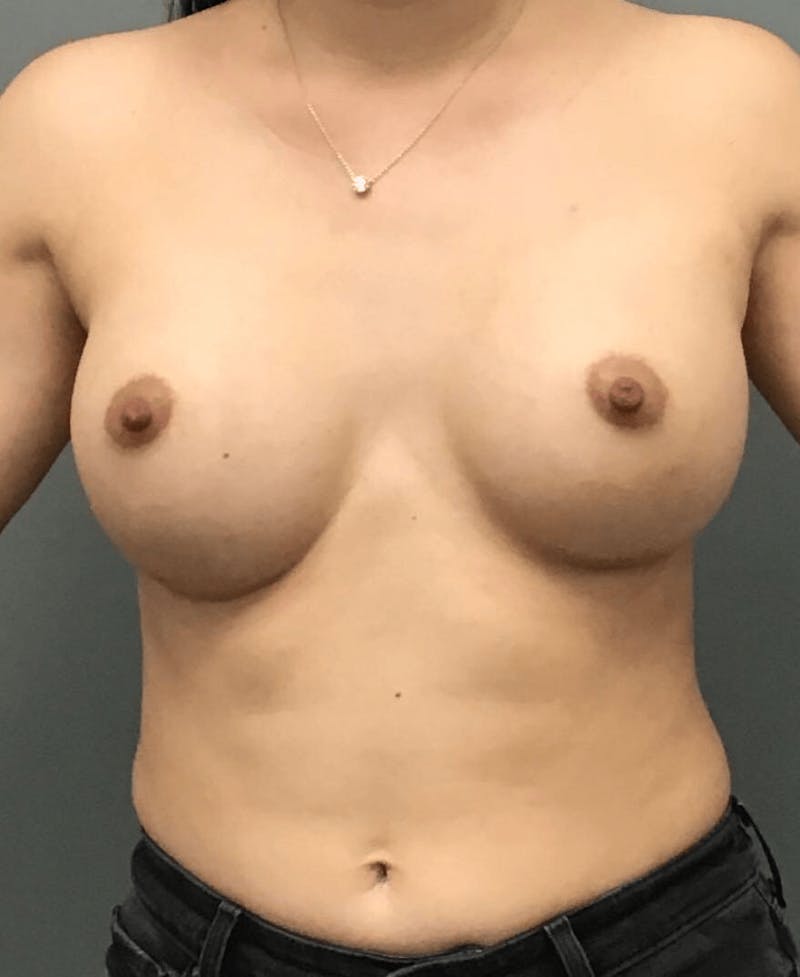
Breast Augmentation Before and After Photo Gallery
Visit Breast Augmentation Gallery for More Before and After PhotosConsidering Aesthetic Options - After Growth Is Complete
Some women choose to address long-standing size concerns, symptoms from heavy tissue, noticeable asymmetry, or changes after pregnancy and weight loss once growth is complete and health is stable. Dr. Baumholtz plans these conversations carefully. He emphasizes proportion over clothing labels by measuring breast base width and considering overall chest shape. Tissue quality informs incision placement, implant style, and whether internal support will help the result last. In most primary augmentations he prefers an inframammary fold incision for precision, with dual-plane placement when it improves contour and softens the upper transition. A Keller Funnel and betadine prep are part of his routine for device handling and sterility. He avoids textured implants and typically selects among smooth devices from Allergan or Motiva to match goals and tissue characteristics. Absorbable mesh can help in thinner patients, with larger devices, or in revision settings to support the lower pole. Fat transfer has a focused role for small adjustments and edge softening, but it is not a one-to-one substitute for an implant when substantial volume is desired.
Age And Device Notes
Regulatory guidance matters. For primary augmentation under age 22, saline implants are generally recommended. After that age, silicone gel may be considered for its feel and performance characteristics. Regardless of age, selection is individualized and aligned with anatomy, lifestyle, and appropriate follow-up.
Follow-Up For Silicone Implants
Long-term care is part of responsible implant surgery. Dr. Baumholtz counsels patients with silicone gel implants to include periodic imaging in routine maintenance. Ultrasound is often the first step several years after surgery because it is accessible and comfortable. MRI is used when ultrasound is unclear or when symptoms suggest a problem. Saline devices are generally straightforward to assess clinically because a rupture leads to visible volume loss, though imaging is used when needed. Regular follow-up visits review comfort, softness, and symmetry and allow questions as life circumstances change.
What A Consultation Includes
Consultations are conversational and practical. Dr. Baumholtz listens first to understand what bothers the patient most and what they hope to change. The examination looks at size, shape, skin elasticity, stretch marks, nipple position, and chest wall features. He explains what each option can and cannot do, where scars will sit, and what day-to-day recovery looks like for work, exercise, and family responsibilities. Recommendations are aligned with health history, daily demands, military duties when relevant, and plans for pregnancy or significant weight change. No surgeon can guarantee a particular cup size or exact look. Expectations are set within realistic ranges, and if surgery is not the right step or not the right time, he says so. Every procedure carries risks, which are reviewed along with benefits, alternatives, and typical timelines for healing.
Practical Tips For San Antonio Life
Comfort often improves with small, consistent choices. A professional bra fitting during adolescence and again as size stabilizes helps with everyday activity, marching band, drill team, and sports. In the heat and humidity common to San Antonio, breathable fabrics and moisture-wicking layers reduce chafing. Hydration matters, as pre-period tenderness can feel stronger during long outdoor days and often eases with adequate fluids and reasonable salt intake. Sports bras are tools for comfort during movement rather than devices that alter growth. While development is ongoing, discreet inserts can even clothing fit without implying anything about final size.
At A Glance Timeline
Most people first notice changes between late primary school and early high school, beginning with thelarche, or breast budding. Menarche often follows two to three years later. The high school years encompass most visible growth and reshaping. By the end of that period, many find that size and shape are fairly predictable from month to month. In the early 20s, small refinements appear as cycles stabilize and body composition settles. Later variations are typically tied to weight, pregnancy, lactation, contraception, and menopause rather than ongoing pubertal growth.
Myths And Facts
Popular advice often misses the biology. Tight clothing, uniforms, or corsets cannot halt breast growth and at most leave temporary marks. Foods, teas, or over-the-counter supplements do not permanently increase size once development is complete. Strength training improves posture and chest muscle tone but does not enlarge breast tissue. Caffeine and late nights may make pre-period tenderness feel more noticeable yet do not extend the timeline of development. Underwire bras are not harmful when they fit properly. Comfort and correct sizing are what matter.
Glossary
The areola is the naturally darker skin that surrounds the nipple. The breast bud, or thelarche, is the earliest palpable sign of development beneath the nipple and areola. Glandular tissue refers to the milk-producing structures that expand under the influence of estrogen and progesterone. The inframammary fold is the crease where the lower breast meets the chest and is often used for precise incision placement. Dual-plane implant positioning places the upper portion of the device under the pectoral muscle and the lower portion under breast tissue to improve contour in selected patients. Menarche is the first menstrual period and commonly appears two to three years after thelarche.
How Dr. Baumholtz Evaluates Asymmetry - Once Growth Is Complete
Assessment begins with a careful history covering timing and pace of change, pregnancies, breastfeeding, weight fluctuations, and medications. Examination looks beyond cup labels to measure base width, assess skin elasticity, note any thin areas or stretch marks, and consider chest wall shape. When a procedure is appropriate, options are matched to the specific imbalance rather than a number on a size chart. A subtle reduction on the larger side can harmonize volume, a small implant on the smaller side can restore projection, and selective fat transfer can soften edges or fill a shallow area. In thinner tissues or revision settings, absorbable mesh can offer internal support to help maintain position. The endpoint is balance that suits the patient’s frame and daily life.
Risks And Limitations
Every operation involves risk, and understanding those risks is part of informed consent. Depending on the procedure, potential issues include bleeding, infection, delayed healing, visible or thickened scars, changes in nipple sensation, fluid accumulation, capsular contracture around an implant, device issues that might require replacement, persistent asymmetry, and the possibility of revision. Dr. Baumholtz discusses these points in detail, along with alternatives to surgery and what can be expected from recovery and long-term maintenance.
Recovery Snapshots
Recovery depends on the operation and the individual. After augmentation, many return to desk-based work within the first week and avoid heavy lifting or chest-dominant exercise until cleared. Lifts and reductions generally bring more swelling and require closer attention to incision care, so time away from work is often longer and activity increases are staged. When fat transfer is used as an adjunct, bruising and swelling can appear at both the donor area and the breast. Compression garments and gentle movement are part of early care. Written instructions and scheduled follow-ups support a steady return to routine.
Imaging And Long-Term Follow-Up
Imaging is tailored to the device and the patient. For silicone gel implants, ultrasound is commonly used several years after surgery as an initial screen, with MRI reserved for unclear findings or specific symptoms. Saline implants are usually obvious when they fail because volume loss is visible, though imaging can still be useful in certain situations. Long-term follow-up visits review comfort, softness, and symmetry and provide a consistent point of contact for questions as bodies and lifestyles change.
Preparing For A Consultation
Arrive with a concise summary of concerns and goals so the conversation stays focused. Bring a list of medications, allergies, and prior surgeries, as well as notes about recent weight changes, pregnancies, and breastfeeding. If previous imaging exists, reports or discs are helpful. Some patients take simple, well-lit photos from the front and sides to document stability over months. During the visit, expect a straightforward discussion of surgical and nonsurgical paths, timelines that fit real life, and a plan that reflects anatomy and priorities. No guarantees are made. The emphasis is on what can be achieved safely and how to care for the result.
FAQs About Normal Breast Development
One breast is bigger in middle school - is that normal?
Yes. Asymmetry is common during puberty. If the difference is extreme or there is a hard lump, discharge, or skin change, see a clinician.
Development started at 9 - is that a problem?
Not necessarily. Many start between 8 and 13. Very early changes before 7 to 8 or very fast changes should be evaluated by a pediatrician or adolescent specialist.
I am 14 and still flat - should I worry?
A small delay can be normal. If there is no breast bud by about 13, clinicians typically evaluate for delayed puberty.
My period started two years ago and there has not been much change - are they done?
For many, most growth occurs within a few years of the first period. If height and bra size are steady, growth may be near complete. Modest changes can still occur into the late teens and early 20s.
Do tight uniforms, sports bras, or even corsets affect growth?
No. Clothing does not change the biology of development. It may leave marks or cause temporary swelling but will not alter final size.
I started birth control and my breasts seem fuller. Is that permanent?
Fullness is often temporary due to fluid and hormone shifts and may settle with time or a method change.
I lost a lot of weight and now my breasts are smaller and sit lower. Why?
Breasts contain fat. With weight loss, volume often drops and the skin can look looser. That is common after large or rapid weight change.
After breastfeeding, one side sits lower than the other. What now?
Post lactation changes are often uneven. If family planning is complete and the difference bothers you, options like lift, reduction, or augmentation can be discussed after evaluation.
What if I feel a new lump?
Most teen lumps are benign, such as fibroadenomas, but any new hard, fixed, or rapidly growing lump should be checked by a clinician.
When do screening mammograms start?
For average risk women in the United States, screening typically starts in adulthood per national guidelines. Family history or high risk factors may change timing. Discuss this with your primary clinician. This page is general education, not individualized screening advice.
Medical References
- Development of the Human Breast. PMC - PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC3706056/
- Breast development in preteen and teenage girls. Texas Children's Hospital. https://www.texaschildrens.org/content/conditions/breast-development
- Etiology of Breast Development and Asymmetry. CORE Scholar. https://corescholar.libraries.wright.edu/cgi/viewcontent.cgi?article=1258&context=bie
- Breast development and disorders in children and adolescents. ScienceDirect. https://www.sciencedirect.com/science/article/abs/pii/S1538544223000901
- Onset of Breast Development in a Longitudinal Cohort. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC3838525/
- Breast Development in Transwomen After 1 Year of Cross-Sex Hormone Therapy. Oxford Academic. https://academic.oup.com/jcem/article/103/2/532/4642966
- Precocious puberty - Symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/precocious-puberty/symptoms-causes/syc-20351811
Ready For A Thoughtful Conversation
Women and families from San Antonio and the Hill Country see Dr. Baumholtz for careful education and long-term follow-up - from the confusion of puberty to changes after pregnancy and through midlife. If you want to know whether development is on track - or you are considering an aesthetic change now that growth is complete - his practice offers a respectful, low-pressure visit.
Phone: 210-660-5579
Email: info@bplasticsurgery.com
You can also request a consultation online and ask to meet with Dr. Michael Baumholtz in San Antonio, TX.